Neuromodulation therapies involve the use of medication or technology to alter pain signaling in the body, aiming to reduce pain and improve overall quality of life. These therapies can be categorized into non-invasive and invasive methods, with applications in treating chronic pain, movement disorders, epilepsy, depression, and anxiety. Techniques include transcutaneous electrical nerve stimulation (TENS), spinal cord stimulators, and emerging methods like deep brain stimulation (DBS) and transcranial magnetic stimulation (TMS). Neuromodulation offers a promising approach to managing various neurological and chronic conditions.
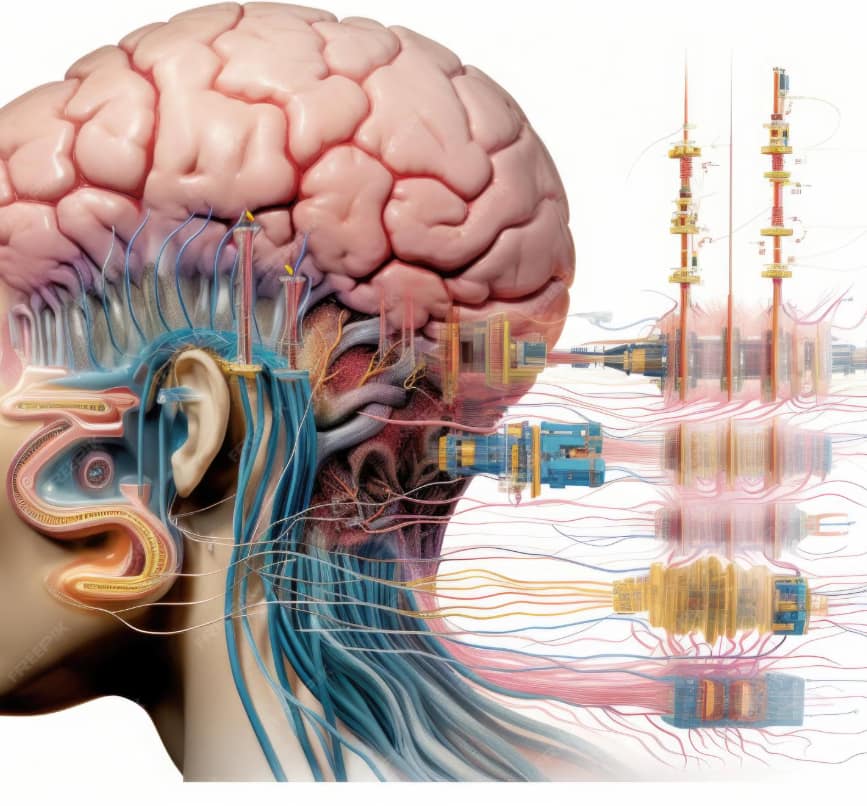
Neuromodulation therapies involve the use of technology to directly influence nervous system activity, aiming to treat psychiatric and neurological conditions. These therapies are especially promising for treatment-resistant disorders. Here are the key approaches and their details:
1. Repetitive Transcranial Magnetic Stimulation (rTMS)
Mechanism:
- Uses magnetic fields to stimulate specific brain regions non-invasively.
- A magnetic coil placed near the scalp delivers electromagnetic pulses to target brain areas, such as the prefrontal cortex.
Applications:
- Major depressive disorder (MDD), particularly treatment-resistant depression.
- Obsessive-compulsive disorder (OCD).
- PTSD and generalized anxiety disorder (GAD) in experimental stages.
Advantages:
- Non-invasive and well-tolerated.
- Minimal side effects, typically limited to mild headaches or discomfort at the stimulation site.
Challenges:
- Limited access due to the cost of equipment.
- Requires multiple sessions over several weeks.
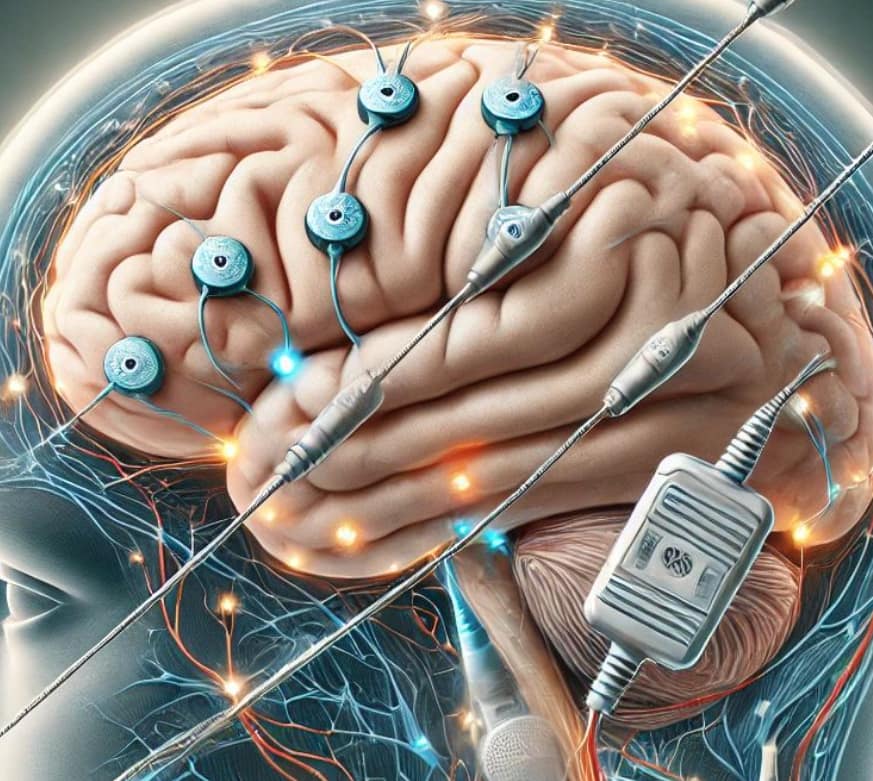
2. Deep Brain Stimulation (DBS)
Mechanism:
- Involves the surgical implantation of electrodes into specific brain regions.
- A pulse generator implanted in the chest sends electrical signals to modulate neural activity.
Applications:
- Initially developed for movement disorders like Parkinson’s disease.
- Expanded to treatment-resistant depression, OCD, and Tourette’s syndrome.
Advantages:
- Precise targeting of brain areas.
- Can provide significant symptom relief for severe cases.
Challenges:
- Invasive with surgical risks such as infection or hemorrhage.
- Requires careful programming and follow-up.
3. Vagus Nerve Stimulation (VNS)
Mechanism:
- Stimulates the vagus nerve through an implanted device in the neck.
- Signals sent via the vagus nerve influence brain areas involved in mood regulation.
Applications:
- Treatment-resistant depression.
- Epilepsy.
Advantages:
- FDA-approved for specific conditions.
- Long-term, low-maintenance therapy once implanted.
Challenges:
- Invasive procedure requiring surgery.
- Side effects like hoarseness, throat pain, or cough.
4. Electroconvulsive Therapy (ECT)
Mechanism:
- Induces controlled seizures using small electric currents applied to the brain under general anesthesia.
- Thought to reset abnormal brain activity.
Applications:
- Severe depression with suicidal ideation.
- Bipolar disorder.
- Schizophrenia (rare cases).
Advantages:
- Rapid symptom relief in severe cases.
- Effective when other treatments fail.
Challenges:
- Potential side effects like memory loss or confusion.
- Stigma associated with its historical use.
5. Transcranial Direct Current Stimulation (tDCS)
Mechanism:
- Delivers a constant, low electric current to the scalp via electrodes.
- Aims to modulate cortical excitability and improve brain function.
Applications:
- Depression.
- Cognitive enhancement in conditions like ADHD or stroke recovery.
Advantages:
- Non-invasive, portable, and inexpensive.
- Fewer side effects compared to ECT or rTMS.
Challenges:
- Less evidence of efficacy compared to rTMS or DBS.
- Standardization of protocols is lacking.
6. Responsive Neurostimulation (RNS)
Mechanism:
- Monitors brain activity in real time and delivers electrical stimulation when abnormal activity is detected.
- Implanted device acts as a closed-loop system.
Applications:
- Epilepsy (FDA-approved).
- Research ongoing for mood disorders and other psychiatric conditions.
Advantages:
- Real-time intervention tailored to patient-specific brain patterns.
- Continuous monitoring provides valuable data.
Challenges:
- Surgical implantation required.
- High cost and complexity.
7. Focused Ultrasound Neuromodulation
Mechanism:
- Uses focused ultrasound waves to stimulate or inhibit specific brain regions non-invasively.
- Often guided by real-time imaging.
Applications:
- Emerging treatment for tremors, depression, and OCD.
- Brain tumors and pain management.
Advantages:
- High precision without surgical risks.
- Non-invasive.
Challenges:
- Limited availability.
- Requires further clinical trials for psychiatric use.
Emerging Trends
- Closed-Loop Systems: Combining real-time monitoring with adaptive stimulation for tailored treatments.
- Combination Therapies: Integrating neuromodulation with pharmacological or psychotherapeutic interventions.
- Neurofeedback Integration: Using brain activity data to enable self-regulation of neural activity.
Neuromodulation therapies are increasingly recognized as powerful tools in modern psychiatry, providing hope for patients unresponsive to traditional methods. However, accessibility, cost, and long-term efficacy remain areas of active research and development.